A Defining Step Toward Whole-Person Health: CMS Advances Oral Health Integration in the 2026 Physician Fee Schedule
Written By the Santa Fe Group (SFG) and the Coalition for Oral Health Policy (COHP)
A Milestone Years in the Making
The Centers for Medicare & Medicaid Services (CMS) has taken a landmark step in aligning federal health policy with an essential truth: oral health is fundamental to overall health.
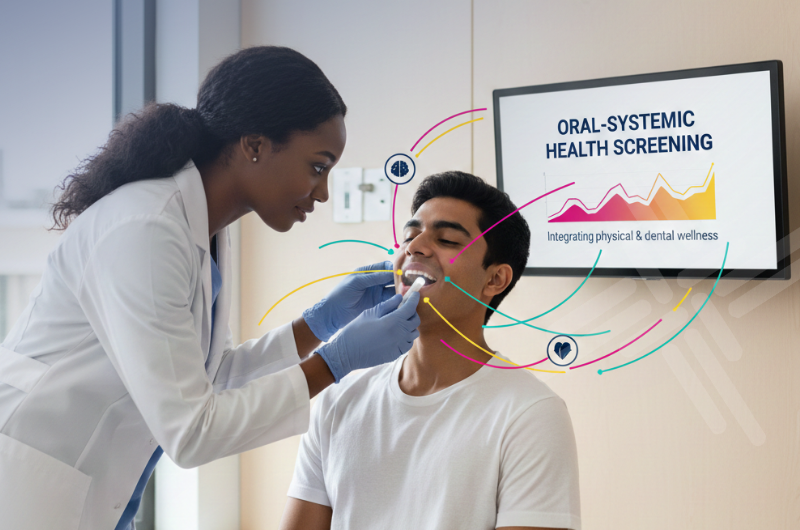
In the Calendar Year 2026 Medicare Physician Fee Schedule (PFS) Final Rule, CMS formally introduced a new Merit-based Incentive Payment System (MIPS) Improvement Activity designed to integrate oral health into primary care practice.
For the first time in the history of the Medicare MIPS program, physicians and other eligible clinicians will be recognized and rewarded for incorporating oral health screening, counseling, and referral into their daily workflow—a structural acknowledgment that the mouth is part of the body and that oral health must be addressed within the continuum of primary care.
What the Policy Does
The new Improvement Activity creates a practical and measurable pathway for integration. Under this provision, clinicians can earn MIPS credit by:
- Conducting oral-health risk assessments and intraoral screenings as part of comprehensive primary care encounters;
- Providing education and counseling to patients about oral hygiene and the oral–systemic connection; and
- Making referrals to dental care for patients who lack a dental home or present with oral-health concerns/problems.
To qualify, clinicians must complete two free online training modules through the Smiles for Life national curriculum—“The Oral Examination” and “Geriatric Oral Health”—and implement practice-based steps such as integrating oral health questions into intake forms, including an oral assessment, updating electronic health-record templates, and establishing referral networks to dental providers.
This Improvement Activity takes effect January 1, 2026, as part of the broader CMS Quality Payment Program (QPP) framework that promotes quality, prevention, and coordinated care.
Why It Matters
This action represents a meaningful and deliberate evolution in federal recognition. Complementing the long-sought dental coverage that has been achieved in recent years for specific medical contexts, this marks the first time oral health has been embedded within a physician performance category tied to value-based payment.
By doing so, CMS is:
- Elevating oral health to a national quality performance priority, placing it alongside other recognized components of preventive care;
- Encouraging collaboration between primary care clinicians and dental providers, creating new bridges across historically divided systems; and
- Laying groundwork for future benefit design, in which oral health is viewed not as an optional add-on but as integral to population health improvement.
This step validates decades of advocacy from public health leaders, professional organizations, and coalitions—such as the Santa Fe Group (SFG), Coalition for Oral Health Policy (COHP), Consortium for Medically Necessary Oral Health Coverage, Center for Medicare Advocacy (CMA), and many others—who have worked to ensure that federal policy reflects the science linking oral and systemic health.
From Siloes to Systems
The introduction of this quality Improvement Activity should be seen as a structural opening—a bridge between policy intention and clinical action. It gives primary care teams the tools, the incentive, and the accountability to bring oral health into everyday practice.
It also demonstrates that integration is a process, not an event. Meaningful change comes through iterative, evidence-driven steps: first, acknowledging the link between systems; next, creating performance expectations; then aligning education, payment, and data to make those expectations sustainable.
In many ways, this mirrors the Santa Fe Group’s long-standing philosophy: achieve systemic transformation through stepwise, achievable reforms that accumulate into lasting impact.
Catalyzing Broader Policy Alignment
This policy shift opens several pathways for deeper integration:
1. Measurement and Evaluation
- The new Improvement Activity offers an opportunity to collect data on screening rates, referral patterns, and outcomes. These metrics can inform future decisions on quality measures, performance benchmarks, and value-based payment models.
2. Health Information Exchange (HIE) and Data Interoperability
- Effective integration requires data systems that communicate across settings. As clinicians begin documenting oral health assessments within medical EHRs, interoperability standards must evolve to capture, share, and analyze oral health data seamlessly across care teams.
3. Workforce Preparation and Interprofessional Training
- The Smiles for Life modules represent a strong start, but should embed oral-systemic content, such as integrating the HEENOT approach to oral exams in medical, dental, nursing, and allied health education. Preparing clinicians for integrated, team-based care is essential for sustainability.
4. Payment and Coverage Evolution
- The Improvement Activity strengthens the case for further coverage reforms. By demonstrating the feasibility and value of oral health integration, it provides the evidence base for expanding medically necessary dental benefits and preventive coverage under Medicare and other programs.
A Success of Partnership and Persistence
This achievement reflects the power of collaborative, multi-stakeholder advocacy. The Santa Fe Group, COHP, and Consortium, working alongside partners in public health, policy, academia, and clinical practice, have long advanced the vision that oral health should be inseparable from health policy, payment design, clinical education, and ultimately, clinical practice.
Through dialogue with CMS, testimony to federal advisory bodies, and sustained coalition work, the community has built the case for integration step by step—grounded in data, feasibility, and patient need.
CMS’s adoption of this Improvement Activity demonstrates that this stepwise approach works: targeted, evidence-based recommendations can translate into meaningful policy change.
Sustaining Momentum: What Comes Next
The next challenge—and opportunity—is implementation. To maintain momentum, stakeholders must:
- Support clinicians and staff with technical assistance (TA), training, and referral tools to operationalize this activity in diverse practice settings;
- Strengthen networks between medical and dental providers to ensure that referrals result in completed care and closed feedback loops;
- Invest in evaluation, documenting impact on health outcomes, chronic disease management, and cost savings; and
- Continue policy engagement to advance complementary reforms that align benefits, incentives, and infrastructure across federal programs.
The Santa Fe Group remains committed to partnering with CMS, HRSA, and allied organizations to monitor progress, disseminate best practices, and identify the next set of actionable opportunities to expand oral-health integration.
Toward a Whole-Person Health Future
With this step, CMS has sent a clear message: oral health is not peripheral to overall health—it is foundational.
By bringing oral health into the Medicare performance framework, CMS has given shape to the vision long shared by clinicians, educators, and policymakers: a system where prevention and integration replace fragmentation and omission.
This policy milestone is both a validation of collective effort and a call to continued action. The Santa Fe Group, COHP, and Consortium applaud CMS’s leadership and invite all partners across the health ecosystem to build upon this foundation—transforming a single improvement activity into a sustained movement toward comprehensive, equitable, whole-person care.
Learn More
- CMS CY 2026 Medicare Physician Fee Schedule Final Rule Summary
- CMS Quality Payment Program 2026 Fact Sheet and Policy Comparison Table (jump to page 36)
- ADA News: CMS Highlights Medical–Dental Integration in 2026 Fee Schedule

Our company (Referral Conduit, LLC™) with 2 patents pending, has developed the CLOSED Loop™ Referral system that supports medical providers referring to dental providers. Our tool includes a complete NPI dental database to support medical referrals to dental providers in your patient’s geographic area. Our dental providers are prepared and equipped to provide the required documentation needed by Medicare CMS MIPS to prove a closed loop referral with Referral Conduit™.
We also support clinician instruction and consulting for your medical and dental teams to implement our Closed Loop™ framework and referral system in your clinical and non-clinical team environments. Please let me know if we can be of further assistance in the oral systemic Medicare initiative.
Thank you.
Dear SFG,
Our company (GSX Pharma LLC) is developing a robust visual oral health screening system that uses visual comparisons to recognize and record oral health/disease findings on an iPad. We are pleased to offer a tool for all trained health care professionals to perform accurate oral health screenings to assist the incorporation of oral health into overall health.
We can demonstrate the preliminary program if desired.
Please advise,